Many people are aware of the risk of skin cancer, especially melanoma, but they may not think to protect or inspect certain areas of the body. Some body parts are more prone to melanoma than others, but skin cancer can occur wherever you have skin—even areas that are often covered and out of sight. One such area is the feet.
Read on to learn more about this condition.
The Basics of Foot Melanoma
As the most dangerous form of skin cancers, melanoma can occur on all parts of the extremities, including hands, feet, and even under the fingernails and toenails. Foot melanoma, also known as acral lentiginous melanoma (ALM), appears on the soles of the feet. Although it accounts for just 1 percent to 3 percent of all melanomas, ALM has disproportionally high morbidity and mortality due to its unusual location and a general lack of awareness. After all, most people don't associate the bottom of the foot with skin cancer. As a result, ALM often goes unnoticed or undiagnosed until it develops into a severe problem that requires more drastic treatment.
Who Gets Foot Melanoma and Why?
Although this type of melanoma affects all people equally once it takes root, it is one of the few types of skin cancers more commonly seen in people of color. In general, fair skin is at high risk for sun-induced skin damage whereas dark, melanin-rich skin is less prone to sun damage and skin cancer. Oddly, though, ALM is usually not associated with sun exposure. Dermatologists and researchers are still unsure of the exact causes, but they know that the condition can arise from normal skin or preexisting moles.
Ethnicity and skin tone aside, this condition affects men and women equally, but it is most common in those over the age of 40. For individuals with a prior history of melanoma, there is an increased risk for ALM on the body.
Identifying Foot Melanoma
ALM can present as an irregular dark patch on the palms or soles (or as a dark line running along the nail plate, in the case of subungual melanoma). It often will contain variations in color. Look for a mixture of blue, grey, red, and dark brown, with asymmetric borders, commonly bigger than 6 millimeters in size. Melanoma in this area is sometimes confused with bruising or blisters, so it's important to track the site over time. If left untreated, the growth will progressively enlarge, change in shape and even ulcerate, or become an open sore.
Although someone with foot melanoma might not be able to feel it at first, they may experience pain, itching, or bleeding as the case becomes more severe.
A Dermatologist can often identify ALM with a visual examination, although they may want to perform one of several types of biopsies to confirm, even looking into lymph nodes to monitor the spread of cancer.
Treating and Preventing Foot Melanoma
Treatment for ALM depends on the depth of the melanoma. Doctors often perform a wide local excision to remove the tumor, removing as little tissue as they deem safe. If caught in the earliest stages, the impact on the patient's everyday life can be minimal. Advanced cases, on the other hand, may require more invasive surgery or even in-depth treatments, such as radiation and chemotherapy.
Unfortunately, there is no proven way to prevent ALM. However, routine self-skin checks of these areas are helpful, especially if a person has experienced ALM or other skin cancers before. Regardless, everyone should receive an annual skin check by a board-certified Dermatologist to catch damage early, whether from sunburns, tanning bed use, or an unknown cause.
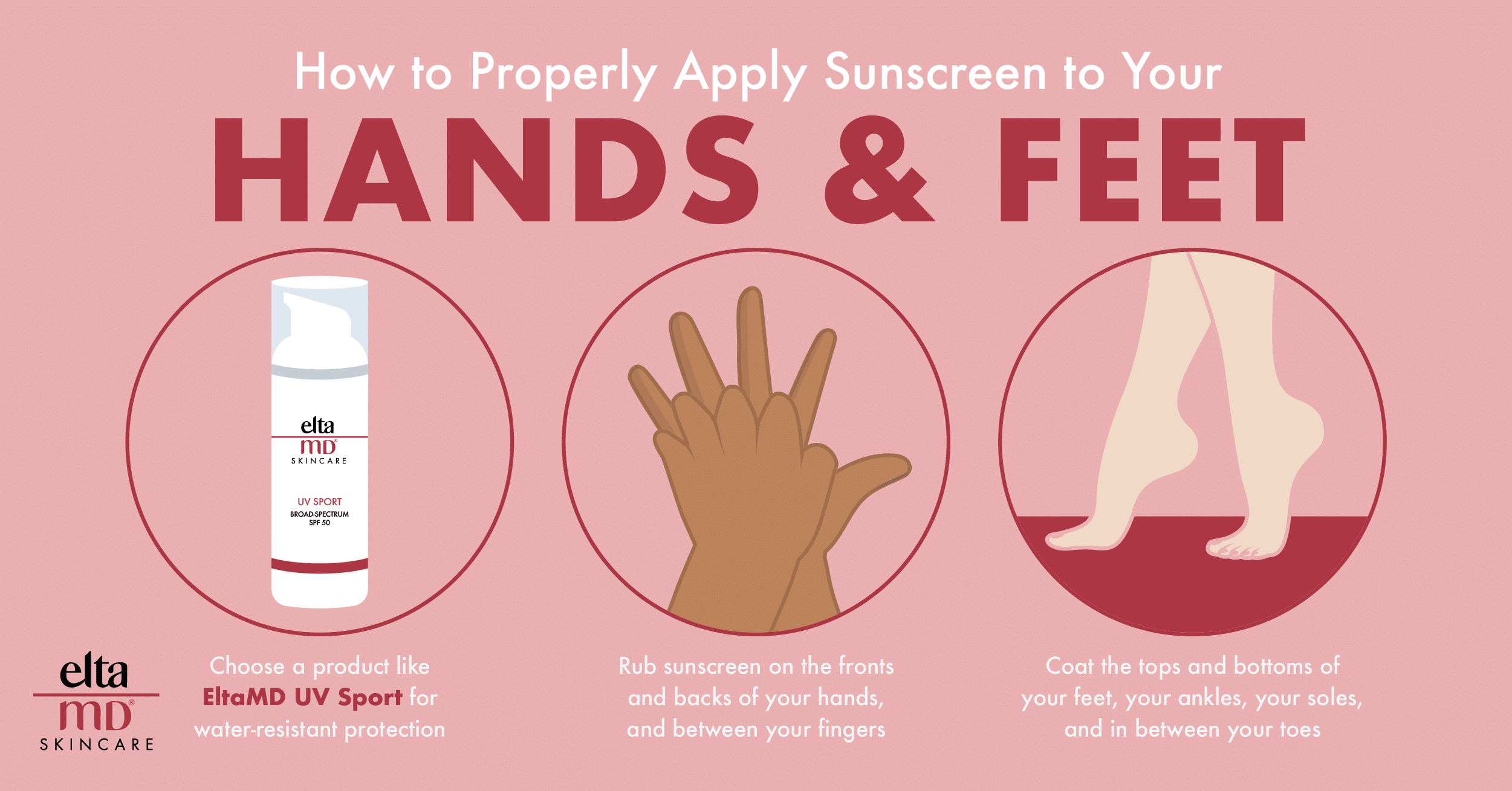
For melanoma elsewhere on the body, your best bet for prevention is the daily use of a broad-spectrum sunscreen with an SPF of 30 or more. Protection with and reapplication of a high-quality SPF product becomes especially important when spending time outdoors and in the water.
Turn to a Derm
Although self-checks and research may be able to help you identify problems early, there is no substitute for an assessment by a trained professional. Remember, if you spot something on your skin and you have any reason whatsoever to believe it's abnormal, the safest path forward is to get it examined. It could be nothing, but this due diligence may well save you from a more painful treatment later—or even save your life.