Skin cancer can occur anywhere on your skin, even places you wouldn't necessarily consider "exposed." Interestingly, this includes under your nails. Although far less common than areas such as the face, arms, and legs, melanoma under nails can be just as problematic as when situated elsewhere on the body and, in fact, can be especially risky, given that it's often noticed and diagnosed later than it might be in more obvious areas.
Read on to learn more about this lesser-known skin cancer danger.
The Basics on Under-Nail Melanoma
Nail melanoma, also known as subungual melanoma, is rare. Of all melanoma locations, the incidence of melanoma in the nail unit is about 2 percent of all melanoma cases. Although the incidence of melanoma is the highest in white men over age 50, subungual melanoma is more common in people of color and, interestingly, is often not associated with sun exposure.
Cancer situated under a finger or toenail can often be overlooked. Even sun-conscious people might not be aware of this somewhat unusual type of cancer, and even if they do notice the characteristic discoloration, they might assume it's some sort of bruising or other nail condition. The under-recognized nature of this condition too often leads to late diagnosis and poor prognosis.
Recognizing Melanoma Under a Fingernail or Toenail
There are four different types of melanoma: superficial spreading, nodular, lentigo maligna, and acral lentiginous melanoma.
Acral (meaning belonging to the extremities) lentiginous melanoma is used to describe melanoma of the nail unit and locations such as the hands and feet. On the palms and soles of the feet, it often presents as an irregularly shaped and colored spot. Under the nail, it can look like this as well, but also commonly appears as a dark line or group of streaks that run down the nail plate originating from the cuticle. As mentioned previously, this can commonly be missed or mistaken for nail trauma.
Treatment for Melanoma Under Nails
Proper treatment involves a Dermatologist performing a biopsy—that is, removing some of the suspect tissue and examining and testing it. This can confirm whether the issue is cancer and determine the depth of growth. If cancer is confirmed, surgical excision will be necessary. Doctors will try to remove as little of the nail and finger or toe as possible and will advise patients on exactly what further treatment or therapy may be needed after the procedure.
For more advanced cases, chemotherapy, radiation therapy, and other in-depth treatments may be used.
After experiencing this type of cancer, it is recommended that patients receive regular full-body skin checks by a Dermatologist to make sure melanoma does not occur elsewhere on the body, as a top risk factor of future melanoma is a history of the disease.
Prevention and Self-Assessment
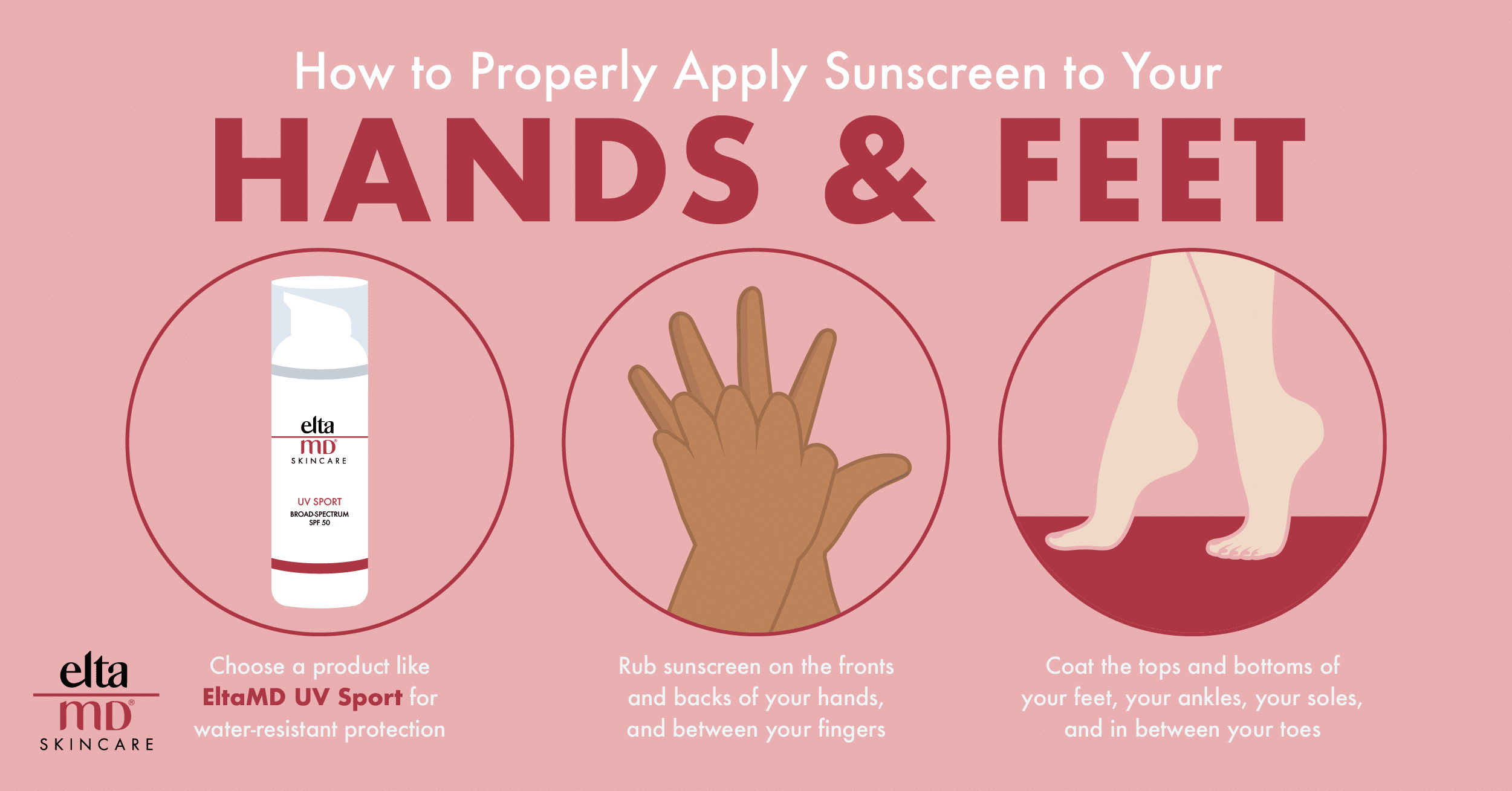
The best way to prevent skin cancer is through proper sun protection and receiving regular skin checks by a board-certified Dermatologist and daily use of a broad-spectrum SPF 30+ sunscreen, sun-protective clothing, and avoiding prolonged direct sun exposure.
Seeing as melanoma under the nails is not strictly linked to sun exposure, Dermatologists encourage monthly self-checks of the skin to help detect irregular or changing marks that could require a visit with a Derm.
When performing these self-checks, stick to the following "ABCDEF rules" in your nail assessment:
A: Age. Peak risk occurs between 50-70 years of age. That said, you're still at risk from age 20-90.
B: Band size. The band or streaks running down the nail will be greater than 3 mm and dark brown or black in color.
C: Changing rapidly. The appearance of the mark shifts in a relatively short amount of time.
D: Digits involved. The specific digits most likely to be affected include the thumb, followed by the big toe, then the index finger.
E: Extension of pigment into the cuticles or side of the nails. The whole area may begin to appear black, brown, or bruised.
F: Family or personal history of melanoma. You can be genetically predisposed to melanoma, and this condition might not be entirely preventable. The most reliable determinant of your risk levels is family and personal history.
Stay Alert and See a Derm—Now and Always
Armed with this knowledge, be sure to keep an eye on your fingernails and toenails just as you would on the rest of your skin. And remember—if you see anything you even suspect is out of the ordinary, it's a good idea to visit a board-certified Dermatologist and to continue to go in for regular skin and nail exams.
These doctors are here to help you, and they are the best resource in your quest for great skin and nails your whole life through.